GLOBAL TREATMENT
Facial clefts (cleft lip, cleft lip and palate and isolated cleft of the palate) are among the most common congenital malformations.
One baby in 600 to 700 is born with a cleft lip and / or palate. The fact that this malformation is so common can not trivialize it in the eyes of parents. They will welcome their child with legitimate apprehensions and fears about its development and future sequelae. There can indeed be sequelae on the aesthetic and functional levels.
Sequelae and multi-disciplinary treatments
The various sequelae with which this type of malformations may be associated require coordination and organization of care. Only an experienced multi-disciplinary team can guarantee them. This is the case of the CHUV CLP team in Lausanne (Switzerland). One of the reasons for the multi-disciplinary team organization is to bring together specialists in o0rder to optimize the complex treatment of multiple sequelae.
But before coming into action, the team has a duty to provide information. It must provide parents with complete, individualized and, above all, understandable information. Essentially, the information contained in these pages revolves around the activity of the multi-disciplinary team, its functioning, its involvement in the management of sequelae in children and adolescents.
Support
The pediatric surgeon (PhD Dr. A. De Buys-Roessingh) comes into contact with the parents sometimes even before birth when a prenatal ultrasound diagnosis has been established. To support parents and the child, to offer optimal care according to the priorities (objectives) and the requests (subjective), only a multi-disciplinary team will be able to be effective.
This team must involve specialists from all the medical and paramedical disciplines concerned. Each of these specialties will be involved, at one time or another, in the development of infants, young children, adolescents and young adults.
Information
The first needs are needs of information. This can be direct and personal. Information via the Internet, with wide and promising possibilities, is unavoidable but can sometimes cause confusion, because opinions diverge between specialists on a certain number of subjects, such as the technique and the timing of the surgical interventions, the necessity or need for a feeding plate, the timing and concept of orthodontic treatment, the indications for orthognathic surgery, etc…
Baby feeding
If parents and relatives need support and information, the first and main concern of the mother is feeding her baby. For the baby precisely, very early, feeding can be a problem. To cope, it is often necessary to make a feeding plate (Fig.2). This plate will facilitate baby’s feeding during the first months of life, until the surgical closure of the cleft of the lip and palate.
Multi-disciplinary team
Later, the child will have to be followed, like all children, by his pediatrician. At the same time, the multi-disciplinary CLP team will be involved, with the intervention of trained and experienced specialists. The team is involved on two levels: a joint consultation activity (organized at regular intervals) and a direct therapeutic activity (treatment, care and advice delivered directly by the practitioners).
Team work
The advantages of teamwork is multiple, both for the patient, his entourage and especially his parents, as for the various practitioners involved. The CLP anomalies have in common their high frequency, but a great variability characterizes the multiple forms that these malformations can take. This variability in form (at the moment of birth) will logically be associated with a great diversity in the consequences (sequelae) that they may cause. These sequelae affect the anatomy, development, aesthetics and function of the masticator and, beyond, the entire craniofacial complex. The diversity of facial clefts is the subject of another article (heterogeneity).
Feeding and breathing of the baby.
These vital functions must be addressed as a priority. A cleft palate can make sucking and, therefore, feeding the baby (breastfeeding or bottle-feeding) difficult. The clefts lip and palate are virtually unable to provide a seal, due to communication between the oral and nasal cavities. The infant is not able to produce the vacuum necessary for sucking breast milk.
Pierre Robin Sequence
Breathing can also be difficult, especially for children born with an abnormality known as the “Pierre Robin Sequence”, a congenital characterised by a triad: cleft palate, micromandiblc and glossoptosis. (Fig.3). Glossoptosis (hypotonic and bulky tongue) interferes with breathing by its excessive posterior position, obstructing the upper airways in the pharyngeal region. The micromandible (small and retruded mandible) forces the tongue to be positioned behind and above, into the cleft palate, thus interfering with breathing.

Feeding plate
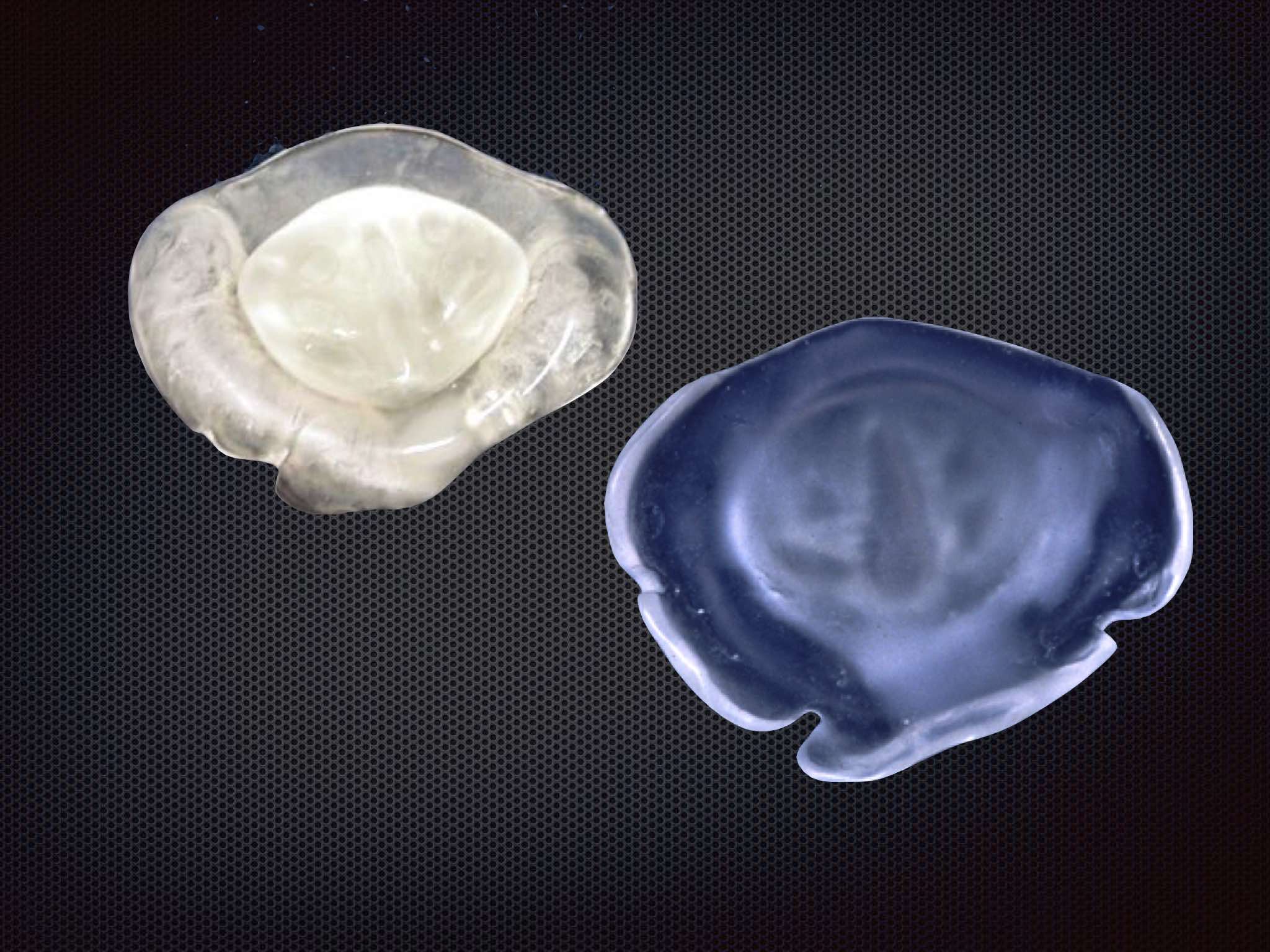
In order to facilitate feeding the baby with a cleft lip and palate, and this from birth on, we recommend the production and fitting of an orthosis commonly called feeding plate or palatal plate. This palatal plate is custom made and it requires the taking of an impression by the orthodontist. This impression is usually done at the hospital, as soon as possible after birth. Indeed, we make every effort to do it the very day of birth, to comfort the parents and allow their baby to eat immediately almost normally. The baby gets used to its plate extremely quickly and the handling of this plate does not pose a problem for parents, who quickly master this useful accessory.

The palatal plate (Fig.4) or feeding plate is made of mixed acrylic material (outer part rigid acrylic, inner part, in contact with the mucosa, soft acrylic). It is perfectly adapted to the baby’s palate and the baby gets used to it in a few hours or a few days at most. The feeding plate allows easier feeding, because it serves as an obturator which covers the cleft palate, thus avoiding communication between the oral and nasal cavities.
Primary surgery
The plate fulfills another important role. The first surgical intervention that the baby will undergo is the closing of the posterior palate cleft (soft palate) around the age of 4 months. The fine sutures that will allow this surgical closure are, as one can imagine, very slender and relatively vulnerable. The palatal plate will play an important role in the protection of these sutures against any external aggression (pacifier, fingers, bottle, toys, etc …).
Follow-up after primary surgery
After the second surgery (closing of the anterior palate or hard palate, and closure of the cleft lip), the plate is no longer necessary. The contacts with the team members will be sparse because a regular support is no longer necessary for some time. Routine checks with the pediatrician, pediatric surgeon, orthodontist and ENT may be needed and will be organized.
Multi-disciplinary meetings
Around the age of 6, a first multi-disciplinary meeting will be organized. The whole team will be called to examine the child, determine his needs and plan active therapeutic management, if it is necessary. Multi-disciplinary meetings are an opportunity to set up a periodic report on the child’s state of health and development. For parents, these meetings are an opportunity to express their requests, to ask many questions, to receive individualised information. And also to get to know all the professionals who can help their child.
Speech therapy
The priority of the care of the small child (5-6 years) is on speech. The child will soon enter primary school. An CLP is sometimes associated with problems of speech development, language acquisition. Often a certain degree of nasality is observed. The soft palate, responsible for the physiological closure of the posterior airway, is sometimes unable to ensure this closure when the patient tries to articulate certain sounds. If too much air escapes through the nose, the sounds will be audibly affected.
The soft palate, although being repaired by a conservative and tissue-respectful surgical technique, will have scars that will affect its mobility. In some cases when speech therapy might not be successful, surgery may be considered. An operation, the velo-pharyngo-plasty, might be considered to create a mucosal bridge between the soft palate and the posterior part of the pharynx. Thus, the flow of air expelled to the nasal cavities during the articulation of certain sounds will be significantly reduced. It is during multi-disciplinary meetings that these treatment indications and modalities are discussed. The speech therapist of the multi-disciplinary team participates and may determine the therapeutic indications of the child.
Otorhinolaryngology (ENT)
The facial clefts affect the ENT sphere in various ways and at many levels. The deviations of the nasal septum, which is frequently encountered, can affect breathing. There is an increased risk of otitis (inflammation and infection in the middle ear). Any degree of hearing loss during infancy may have negative or even disastrous consequences on language development and acquisition.
For these reasons, regular controls by the team’s ENT, who is also specialized in audio-phonology, are of paramount importance.
Psychology
Finally, during the development of the child and adolescent, psychological problems related to the physical consequences of his malformation can arise. Difficulties of adaptation, if they are rather rare, remain nonetheless handicapping. Parents themselves may need counseling and psychological support to overcome transient difficulties related to their child’s condition. The psychologist of the team, specialized in the problems of youth and adolescence, will be involved: the parents and / or the child will be able at any time to use his / her advice and therapeutic services.