ORTHODONTICS
Orthodontic management of sequelae of facial clefts
Georges Herzog, orthodontist spéc. SSO.
Orthodontics is one of the specialties of the multi-disciplinary team dealing with the sequelae of palatal, labial, labio-maxillary and labio-maxillo-palatal clefts. All children and adolescents affected by the malformation are followed, assessed regularly on the dental and orthodontic planes and the majority, if not all, will require orthodontic treatment at some point in time during their growth and development.
It should be stated in the preamble that there are as many treatment concepts as active teams. This has been highlighted by numerous studies and surveys, such as the community project known as Eurocleft (2001).
Unfortunately, on many points, there is little or no consensus: technique and timing of primary surgical procedures, need and usefulness of a palatal plate (feeding plate) need and timing of alveolar bone graft, indication for early orthopaedic (orthodontic) treatment, need and indications for orthognathic surgical management.
This page does not pretend to be representative or to constitute a sort of method, a system worthy of being recommended and generalized. It simply reflects the vision and treatment concepts of a multi-disciplinary team, based on the experience of the specialists on this team.
The problems encountered vary with the severity of the initial cleft. An isolated cleft of the palate will have less severe consequences than a complete uni- or bi-lateral cleft involving the primary palate and the secondary palate. We will therefore consider first and foremost the orthodontic treatment of complete clefts.
Sequelae of the facial clefts affect the craniofacial complex as a whole. The inter-maxillary relationships are affected by the growth disorders induced by the malformation itself and subsequent deformities, which are largely caused by the scar tissue-related inhibitions that inevitably primary surgery has produced (Fig. 1). This scar tissue intervenes in areas of sensitive growth: the alveolar bone and the supporting tissues of the teeth, the palate, the base of the nose, the soft tissues, etc.
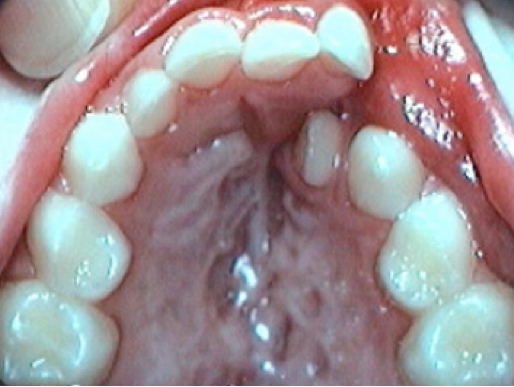
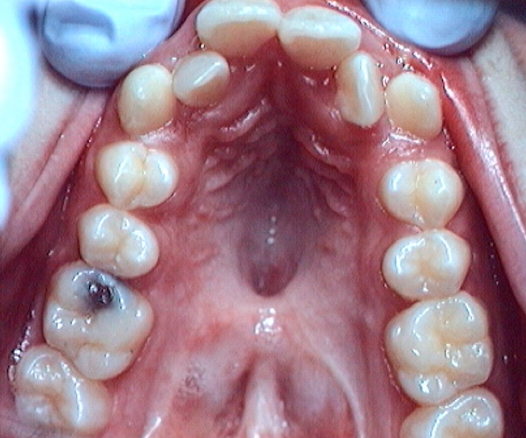
Fig 1 Scar tissue : left, cleft of the lip and palate ; right, isoéated cleft of the palate
From a dental point of view, we are often faced with severe sequelae and the challenges far exceed those of the general population.
We can consider three categories of dental sequelae and cranio-facial clefts:
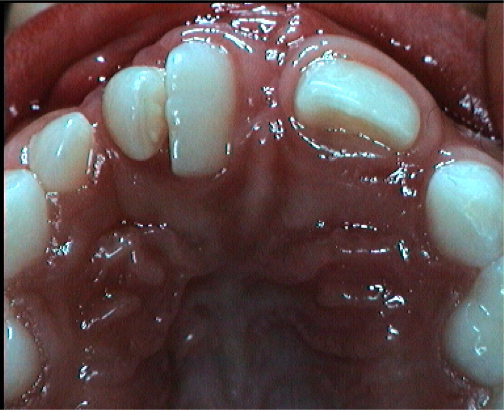
1) Absence of the lateral incisor on the side of the cleft.
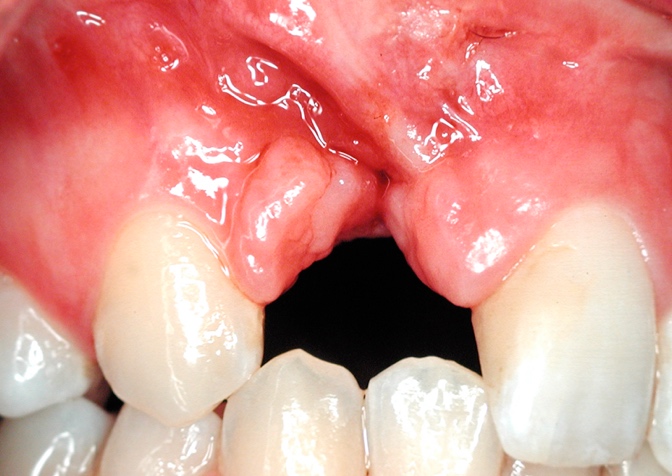 Fig 2. The lateral incisor is absent or malformed in most cases (76%) or has abnormalities of size and / or shape (> 95%). The problem number one is: should we replace this tooth with an implant or rather try to close the space by moving the neighbouring teeth in its place by orthodontic means? One of the most extensively debated topics.
Fig 2. The lateral incisor is absent or malformed in most cases (76%) or has abnormalities of size and / or shape (> 95%). The problem number one is: should we replace this tooth with an implant or rather try to close the space by moving the neighbouring teeth in its place by orthodontic means? One of the most extensively debated topics.
2) growth deficiency of the upper jaw:
The maxilla (upper jaw) is retrognathic, sometimes with vertical growth deficiency also, and the profile of the patient may have a more or less pronounced concavity, highly handicapping from an aesthetic and functional point of view. Inter-maxillary relationships are affected: articulated crossbite and open bite.
 Fig 3 Lateral profile Xray: hypoplasia of the upper jaw and concave profile
Fig 3 Lateral profile Xray: hypoplasia of the upper jaw and concave profile
3) Dental malpositions:
Fig 4 Dental malpositions : rotations, crossbite, lack of space
The effectiveness of complex orthodontic treatment depends on many factors, but therapeutic methods based on scientific evidence must be used, according to a controlled intervention schedule. We must act in a timely manner, taking into account all the parameters with a long-term vision. A therapeutic calendar is applied in a systematic way, at least in its main lines, while remaining individualizable:
CALENDAR AND GENERAL CONCEPT OF ORTHODONTIC MANAGEMENT:
- Creation of a palatal (feeding) plate from birth to 6-8 months following the primary surgical schedule (Fig 5)
- Deciduous dentition: no treatment; conservative dental follow-up.
- Alveolar cleft: if necessary: palatal expansion followed by alveolar bone graft (GOA); retention.
- Mixed dentition (after GOA): alignment of upper incisors if necessary (objective / subjective)
- Permanent dentition: depends on the prognosis. If orthographic surgery (40 to 60%): delayed orthodontic treatment (16-17 years).
If the prognosis is favorable (that is, orthognathic surgery is not indicated) conventional orthodontic treatment will be planned. If sequelae are severe, this should not necessarily imply early management and continuous treatment. On the contrary: one should not impose a too heavy (long) therapeutic burden on patients who have to undergo other treatments as part of multi-disciplinary care.
The principle of efficiency must be incorporated into treatment planning. Efficiency is efficacy obtained with an economy of means.
Georges Herzog, consultant orthodontist of the multi-disciplinary CLP team at CHUV (Lausanne) and HUG (Geneva)
contact: info@cleft-palate.com